Clinical Application of a Shape Memory Implant Abutment System

Contents
Abstract
An innovative abutment system has recently been developed to address the well-known limitations of screw- and cement-retained implant restorations. This abutment system offers retrievability by replacing the cement layer with a precision-engineered nickel-titanium sleeve that switches between shapes that lock and unlock the prosthesis. The avoidance of cement precludes cement-related periimplant complications, while the elimination of occlusal screw access holes may enable predictable control over occlusion and improve the structural integrity of the prosthesis. By eliminating the need for cement clean up, occlusal access closure, and occlusal adjustments after insertion, the dentist is afforded more time to attend to the patient’s general needs. This paper describes the design rationale for and clinical treatment using this novel abutment system. (J Prosthet Dent 2017;117:8-12)
Article
Screws and cements are the 2 methods of attaching restorations to dental implants. Screw-retained implant restorations permit a retrievability that, in theory, allows for effortless inspection of underlying components. In practice, screw retrieval is only performed to repair damaged or fractured components because screw removal, reinsertion, and restoration of occlusal holes can be time consuming.1 For multiunit fixed prostheses, screw tightening can induce significant residual stress if passive fit is not achieved between the framework and implants. Furthermore, the composite resin materials covering the screw access holes are prone to wear and do not offer stable control over occlusion.1-4
The most frequently cited complications of screwretained implants include prosthetic screw loosening, fracture, and failure of the prosthetic materials.5-7 Kreissl et al.8 evaluated more than 200 implants over a 5-year period and observed 6.7% screw loosening and 5.7% porcelain fracture. In a systematic review, Zurdo et al.9 reported that over 20% of fixed implant restorations suffered porcelain fracture or screw loosening.10 The lingual set screw approach offers excellent occlusion control but requires additional technical expertise and clinical chair time to properly implement.
Cemented restorations trade retrievability for the elimination of the screw access hole.11 The similarity to conventional fixed restorations, ease of use, and superior esthetics have made cement popular. In addition to better control over occlusion, cement also enables better anterior esthetics and permits a restoration when implant angulation would place the access hole on the labial surface. With cement, a passive fit for multiunit prostheses becomes less critical because the cement fills in the misfit regions between the abutment and the restoration.12
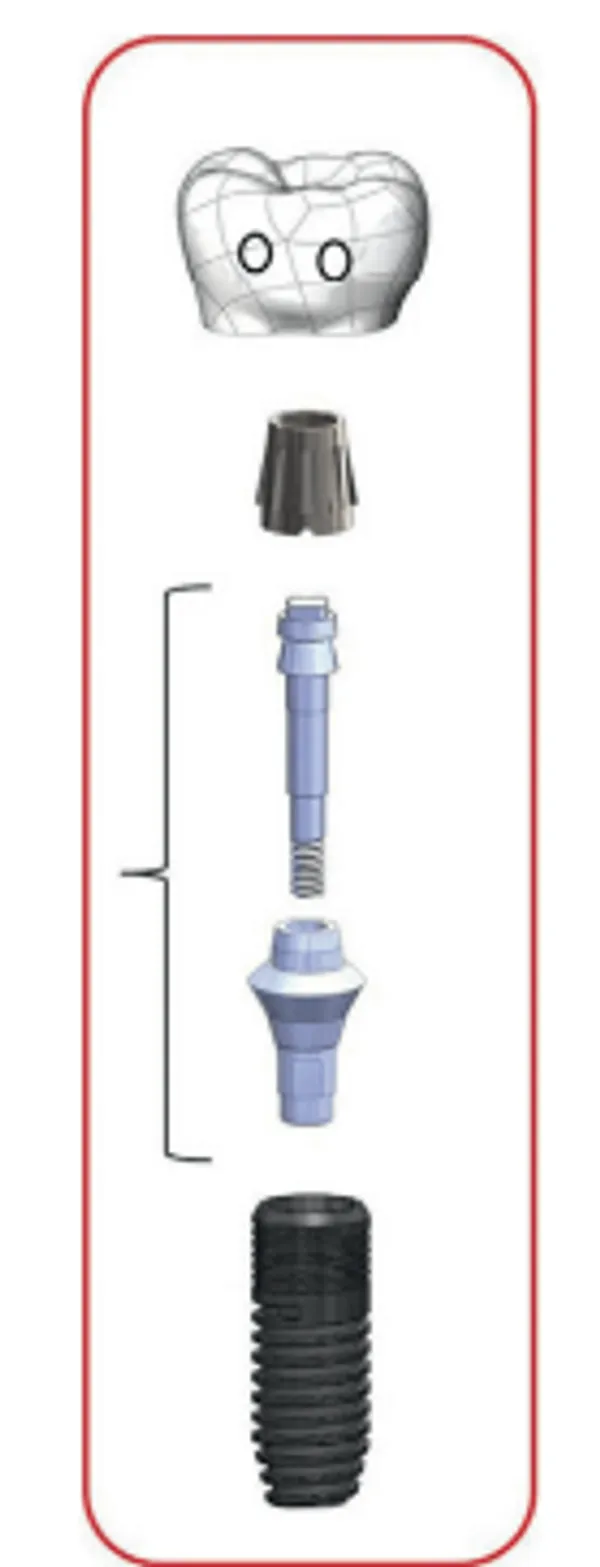 Figure 1. Overall concept of abutment and sleeve system
Figure 1. Overall concept of abutment and sleeve system 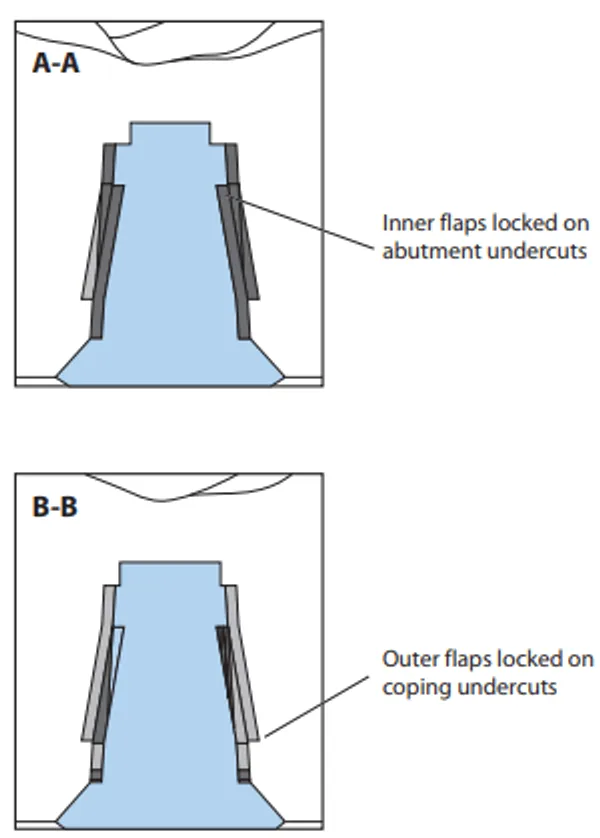 Figure 2. Cross-section view of flaps engaging undercut in abutment and restoration
Figure 2. Cross-section view of flaps engaging undercut in abutment and restoration The principle disadvantages of cemented restorations are irretrievability and subgingival residual cement. The lack of irretrievability precludes high-temperature porcelain repair and the ability to retighten implant abutment screws without drilling through the restoration. During cementation, hydrostatic pressure may prevent the crown from seating completely, resulting in hyperocclusion.13
Cement removal becomes increasingly difficult with increasing subgingival depth. Numerous studies have shown a positive correlation between periimplantitis and the presence of excess cement. Korsch et al.14 reported the presence of residual cement in 60% of cemented restorations. Excess cement was associated with bleeding (80%) and suppuration (21%) around implants. Importantly, the removal of excess cement led to a 77% reduction in bleeding and a 100% reduction in suppuration. Moreover, in a 5-year prospective clinical study, Wilson et al.15 reported a positive correlation between excess cement and periimplant disease. The authors reported that all 42 patients with clinical signs of periimplant disease had excess cement, while excess cement was not found in any of the control healthy patients. After cement removal, 75% of the sites recovered, with no further clinical or endoscopic signs of inflammation.
To address these known complications, a new implant retention technology has been developed to combine the advantages of screw (retrievability) and cement (occlusion, esthetics) while eliminating the disadvantages of composite resins and residual cement. This new system consists of a precision machined abutment that fits onto most commercial dental implant fixtures. The abutment accepts a shape memory sleeve (Smileloc; Rodo Medical) that features 2 sets of movable flaps that switch between the “engaged” and “disengaged” positions that lock and unlock the restoration.
 Figure 3. Occlusal and profile view of Smileloc Sleeve
Figure 3. Occlusal and profile view of Smileloc Sleeve As shown in Figures 1-3, the engaged position locks the crown onto the implant. First, the inner flaps of the sleeve engage with the abutment undercut. When a crown is inserted over the sleeve, the outer flaps engage the coping undercuts, thus connecting the abutment-sleeve-coping into 1 mechanically interlocking system.
To retrieve the restoration, the sleeve is heated through a lingual access hole by a device to induce a shape change that returns all flaps to the disengaged positions, freeing the crown, sleeve and abutment from the undercuts. This loss of mechanical interlock allows the prosthesis to be retrieved with finger pressure. Unlike screws and cements that are subjected to tension during crown removal, in this abutment-sleeveinterlocking system, the force vectors exert mostly compressive stresses on the sleeve. Therefore, the sleeve flap design takes advantage of the fact that most materials are much stronger in compression than in tension.
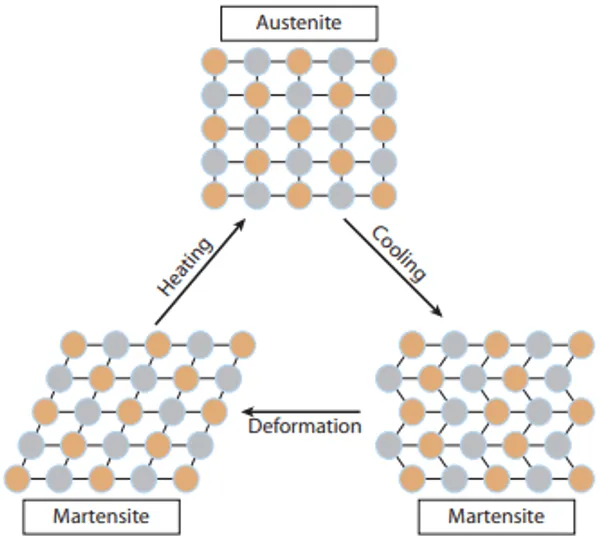 Figure 4. Transfomation phases of nitinol.
Figure 4. Transfomation phases of nitinol.  Figure 5. Implant with abutment in place and retentive sleeve on right along with titanium coping.
Figure 5. Implant with abutment in place and retentive sleeve on right along with titanium coping. The sleeve is made of nitinol, an alloy of nickel and titanium that is commonly used in interventional cardiology devices with well-documented human biocompatibility.16 In dentistry, nitinol orthodontic arch wires and endodontic instruments take advantage of the superelastic properties of nickel-titanium. The solid-state phase transformation, also known as the martensitic transformation, is a reversible process in nitinol. As shown in Figure 4 and 5, the parent phase is the austenite (cubic) phase, and the daughter phase is the martensitic (monoclinic) phase. The austenitic phase is the remembered phase as set by heat tempering during the manufacturing process. Upon cooling, there is a phase change to the martensite phase without any physical change in shape. When an external deformation stress is applied, the phase remains as a martensite phase, but because of the ability of the alloy to undergo twinning, the alloy remains in that deformed shape. Twinning is a unique property of the nitinol alloy. The alloy undergoes limited deformation without breaking any atomic bonds, although there is a rearrangement of the ions without any slip.17
 Figure 6. Abutment analog and titanium coping for crown fabrication. Closed tray snap-on impression coping seating intraorally.
Figure 6. Abutment analog and titanium coping for crown fabrication. Closed tray snap-on impression coping seating intraorally. 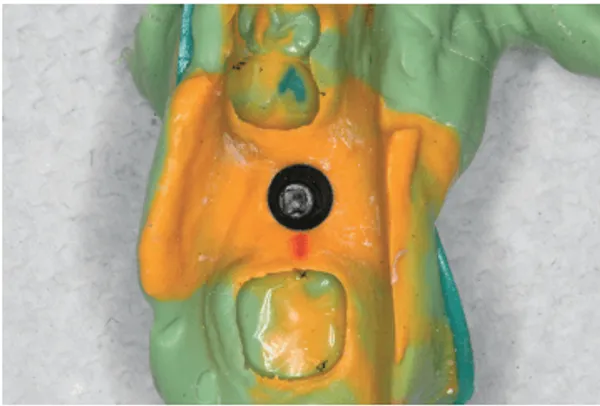 Figure 7. Closed tray polyvinyl siloxane impression.
Figure 7. Closed tray polyvinyl siloxane impression. This abutment design takes advantage of nitinol’s shape memory properties, where the sleeve mechanically deforms to one shape at room temperature and then recovers its original, undeformed shape upon heating to above its transformation temperature. The heat transfer from the abutment to biological tissues, the mechanical resistance to displacement, and the fatigue properties and corrosion resistance of the new abutment system have been studied in detail by the authors and will be published in future reports.
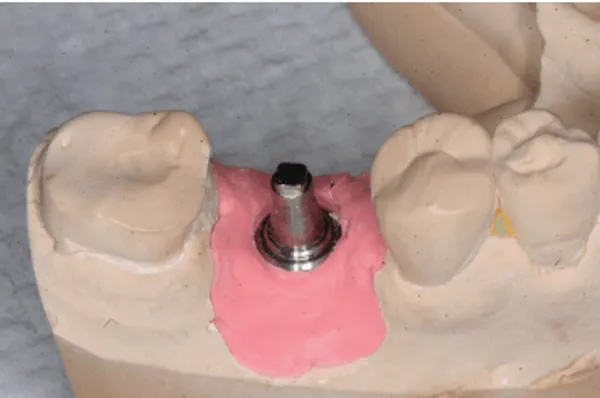 Figure 8. Definitive cast with abutment analog in place.
Figure 8. Definitive cast with abutment analog in place. 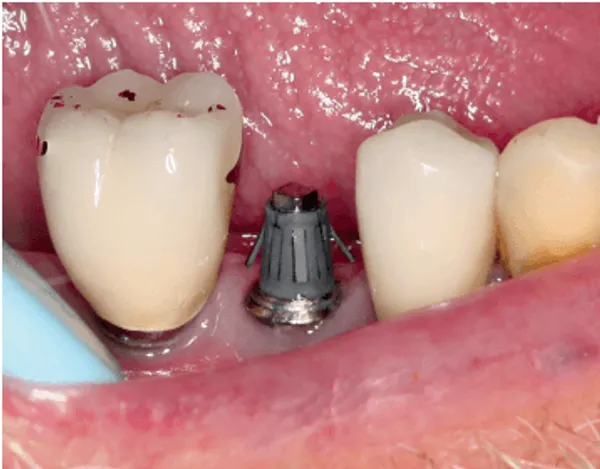 Figure 9. Abutment and retentive sleeve in place intraorally.
Figure 9. Abutment and retentive sleeve in place intraorally.  Figure 10. Implant crown in place. Lingual channels were filled with interim restorative resin plug.
Figure 10. Implant crown in place. Lingual channels were filled with interim restorative resin plug. 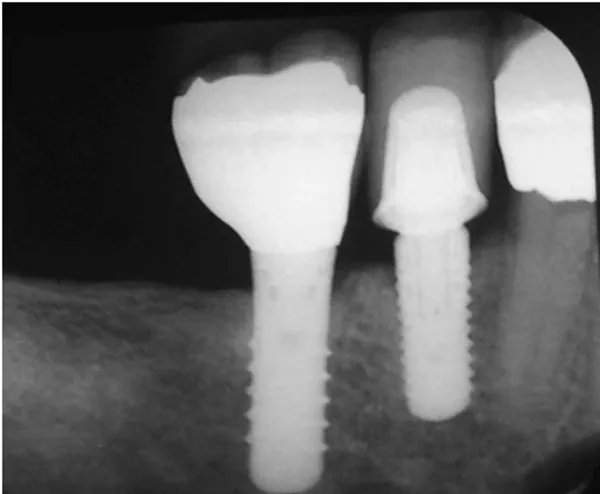 Figure 11. Radiograph of abutment and restoration in place.
Figure 11. Radiograph of abutment and restoration in place. Clinical Report
With approval from the UCLA Institutional Review Board, a patient with a single posterior osseointegrated implant (Replace Tapered; Nobel Biocare) was selected, who consented to the clinical feasibility study of this new abutment system. At the impression appointment, the abutment was tightened to 35 Ncm according to the manufacturer’s instructions. A snap-on impression coping with matching antirotational index was used to make a closed tray polyvinyl siloxane impression. (Figures 6, 7). At the delivery appointment, a metal ceramic crown with precision undercuts in the titanium coping was inspected for proximal contacts, marginal fit, and occlusion (Figures 8-10). The lingual access holes were filled with an interim restorative material (Fermit; Ivoclar Vivadent AG). After adjustment and polishing, a nitinol sleeve (Smileloc) in its engaged position was placed onto the abutment. The crown was then seated with finger pressure and occlusal pressure on a wooden occlusal stick. A periapical radiograph was made to verify seating (Figure 11). Probing depths were recorded with a 6-point system, and the gingival and plaque indexes were noted. A baseline record of the occlusal stability was made with a pressure mapping sensor (T-Scan Evolution System; Tekscan Inc). The stability of the crown was measured with a wireless device (Periotest M; Medizintechnik Guiden e.K) at 3 locations on the length of the restoration. The patient was instructed to function normally and perform routine oral hygiene procedures.
At the end of the institutional review board-approved 6-month observation period, the patient returned for crown removal. Removal was required because this was an investigational study of a medical device prior to U.S. Food and Drug Administration (FDA) clearance. The patient reported no complaints, and no changes were noted in the gingival parameters and occlusal contacts. The crown was stable, with no signs of mobility. Periotest values were similar to initial readings. To remove the crown, the interim restorative material (Fermit; Ivoclar Vivadent AG) was removed from the lingual holes. A microprocessor-controlled activator probe was inserted into the lingual holes to produce direct contact with the titanium coping (Figures 12, 13). During 15 seconds of contact resistive heating, the sleeve flaps changed shape from engage to disengage, thereby allowing the crown and sleeve to be removed from the abutment with finger pressure. Inspection of the removed crown, abutment, and sleeve revealed exceptionally clean interfaces. The tissues appeared healthy, and no clinical signs of inflammation were observed. The probing depths and gingival and plaque indexes remained unchanged from the preinsertion records. Using the data from this feasibility trial, an FDA investigational device exemption (IDE) study is currently ongoing and will be reported when completed.
 Figure 12. Activation device used to retrieve screw-retained crown.
Figure 12. Activation device used to retrieve screw-retained crown.  Figure 13. Close-up of activation tip.
Figure 13. Close-up of activation tip. Summary
This innovative abutment system combines the retrievability of screw-retained abutments with the ease of use, occlusion control, adaptability to implant angulation, and esthetics of cement-retained prostheses. The shape memory abutment eliminates the need for occlusal composite resins and the risk of subgingival residual cement. These distinct advantages justify further detailed investigations, longer clinical evaluation, and more indepth analysis of physical, electrochemical, and biological performance.